Archive for the ‘Uncategorized’ Category
21.8.18
A 45 years old female had reportedly undergone an ERCP attempt to clear the CBD of stones but the stones could not be removed, and a biliary stent was placed. Another endoscopic attempt was made a month later, perhaps with an additional sphincterotomy (no records available, as usual) but ending up with biliary peritonitis (possibly due to a duodenal perforation) which was treated with US guided pigtail catheter drainage. The patient recovered and an MRCP on 2nd August revealed 4 big stones in the bile duct
At open operation, the whole upper abdomen was found to be frozen in postperitonitis adhesions, and the CBD was located with great difficulty, and confirmed with needle aspiration. At choledochotomy, the CBD was found to be clear, with no stones. This was confirmed with choledochoscopy. A T-tube drain was placed. The gallbladder was not found. Postoperatively the patient did very well and remains well.
Why were there no stones in the CBD?? Possible they had passed out through the sphincterotomy!
20.10.18
An obese 40 years old lady, having consulted Columbia Hospital, reported for laparoscopic cholecystectomy. She had elevated serum alkaline phosphatase levels assessed repeatedly over a period of nearly two months, raising a suspicion of CBD stones. However, an MRCP showed no stones and a regular laparoscopic cholecystectomy was done.
Disulfiram implants, a big goitre, a bad splenectomy, a jejunal perforation by a trocar, an STS masquerading as an abscess, and a phyllodes tumor
Posted on: July 6, 2018
8.4.17
Excised two chronic abscess cavities that had formed around disulfiram tablets kept subcutaneously in the anterior abdominal wall in a 55 years old man, for his alcoholic addiction. Patient now reformed and normal and wanted removal of the implants which were causing pain.
I had never heard of such a thing as disulfiram implants. The present case had them implanted in Canada.


24.1.18
Cesarean hysterectomy for placenta accreta and percreta in an 40 years old lady with 12 weeks unwanted pregnancy. Very bloody surgery with large blood loss sending patient into hypotension (caused by the prolonged attempts by the attending gynecologist to manually separate the placenta), but fortunately ended well in the end. The D&C which was being discussed too in the management plan earlier by the gynecologist would have been disastrous.
25.1.18
A big vascular goiter in a 45 years old obese female. Right thyroid lobectomy took nearly three hours.

29.1.18
A lap chole was thrust upon me when Shashi Pathak w/o dr Pathak (microbiology) insisted on it even as she actually had no symptoms pertaining to gallstones. Actually turned out to be primarily suffering from depression for which was later treated by psychiatrists.
24.2.18
Splenectomy for shattered traumatised spleen 25 m. Bad and strange experience in the postoperative period when the patient continued to pour out litres of jejunal fluids through the nasogastric tube, and getting into huge water and electrolyte losses and dehydration. Explored on 1.3.18 to find acutely swollen and matted upper jejunal loops which were separated and washed clean. This did not help and another exploration was performed on 3.3.18 to rule out a mechanical factor in the distal loops. There was no such thing and the patient had to be kept on TPN for more than a week before he recovered. Inexplicable to me. Possibly, the poor anesthesia and poor relaxation caused a lot of bruises over the upper small bowel loops when they were covered with packs and retracted with lot of force. Also the abdominal packs given by the nurse were dry (not moist as they should have been). She said she never uses moist packs!
27.2.18
Another bad experience with a big incisional hernia (following pyelolithotomy) in an elderly 70 years old lady, repaired with a large mesh. Postoperatively developed a big seroma that took long time to heal.
5.3.18
Babaji from Dhanthal gurudwara presented with a hernia for which repair was done in Giani Lal Singh hospital.
6.3.18
A trocar perforation of the jejunum had to be repaired when called upon to do so by dr Vikram Tandon who was doing a lap chole.
7.3.18
Surinder bhahiji’s lap chole, went very well. Rinku had come all the way from New York to watch!
12.3.18
A presumed abscess of the thigh ( huge in size, diagnosed clinically and confirmed on CT scan) drained in an elderly ( 60 years old) female. The fluid was largely serous with lots of flakes. When examined after a month or so, the wound had partially healed but the cavity was filling up with a fleshy growth. Was referred to PGI where a high-grade soft-tissue sarcoma was diagnosed. She died soon after.


16 april to 17 may 2018 visit to America and Canada.
19.6.18
A lap chole for polyp and sludge in the gall bladder.

2.7.18
A big phyllodes tumor in the left breast of a young girl (18 years old) excised.
23.6.17
23 years old hefty young man had a hard small tumor of hard palate. Excised with cautery. Biopsy was benign pleomorphic tumor. Unfortunately developed a small palatal fistula possibly due to overuse of cautery. Had to be repaired by dr Harsimran, the ENT surgeon.
29.6.18
An epulis on left lower gingiva excised from a 55 years old lady turned out to be malignant. Referred to Tata cancer center Sangrur where it was re-excised and the patient remains well till date.
26.7.17
A gangrenous gall bladder excised laparoscopically with great difficulty due to frozen Calot’s triangle. Patient 56 years old male and related to sarpanch of village Chouhat.
10.8.17
Ovarian cancers bilateral excised at a TAH bSOP (dr Jagga’s case).

23.8.17
Attended the free medical camp held by Sarbat da Bhala trust in central jail to examine prisoners.
7.9.17
A badly neglected case of scrotal and testicular gangrene in a young man of 24 years ( referred by dr Sachdeva) explored and the testis had to be removed. Scrotal debridement and closure performed. Healed well.
23.9.17
An open CBD exploration (after failed ERCP attempts) and stone removal along with open cholecystectomy performed after a long time. This appears to me still to be a very satisfying procedure.
1.11.17
Joined VMHC (Vardhman Mahavir healthcare) as part time surgeon for 2 hours (9 to 11 am) everyday except Sunday.
5.12.17
A pilonidal sinus excised and closed in a young teenager male, only to get the wound infected after removal of sutures after 2 weeks and then for the wound to take more than 2 months to heal.
28.12.17
Fournier’s gangrene badly infected and the patient (65 years old man) septic going into MOD, shifted from some delhi hospital, underwent thorough debridement and survived. Scrotal skin could be closed several days later.
The anatomy of Rouviere’s sulcus as seen during laparoscopic cholecystectomy
Posted on: May 14, 2017
https://www.ncbi.nlm.nih.gov/pubmed/28281470
The Rouviere’s sulcus can now be defined in three simple terms – a deep sulcus, or a slit or a scar. We recommend that as a first step in laparoscopic cholecystectomy, the surgeon must look for this reference point (whether it is in the form of a scar, or a slit or a real sulcus) which will be the plane of the main bile duct, and thus avoid any dissection below this point in order to eliminate any danger to the bile duct during surgery.
 The Scar
The Scar
 The Slit
The Slit
 The Sulcus (open)
The Sulcus (open)
 The sulcus (closed)
The sulcus (closed)
22.3.17
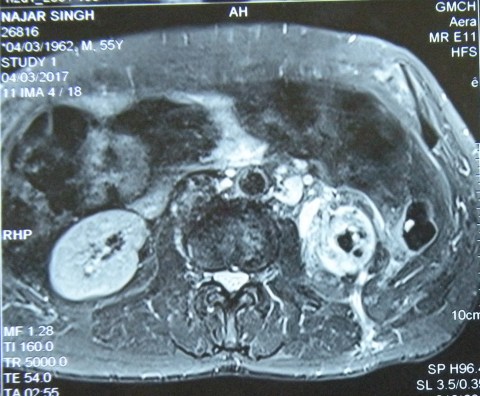
An elderly man (65 years old) presented with a sinus on the back in the loin area, occasionally discharging when the patient passed urine. Investigations revealed a poorly functioning non-salvageable left kidney, and the MRI scan reported xanthogranulomatous pyelonephritis with a nicely outlined fistula through the posterior abdominal wall onto the skin of the back on the left side. A difficult nephrectomy was performed along with excision of the whole fistula tract.


10-13 November, 16
Attended the ICS conference at Guwahati along with dr Sukhpreet, dr Jagga and dr Grover. Also saw dr Bhardwaj there.
21.1.17
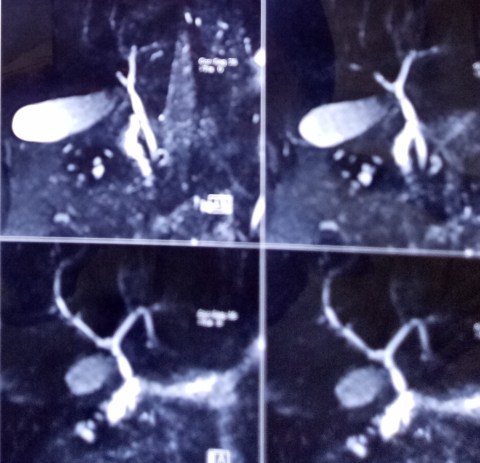
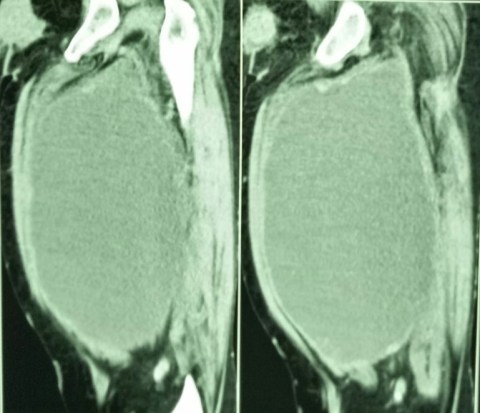
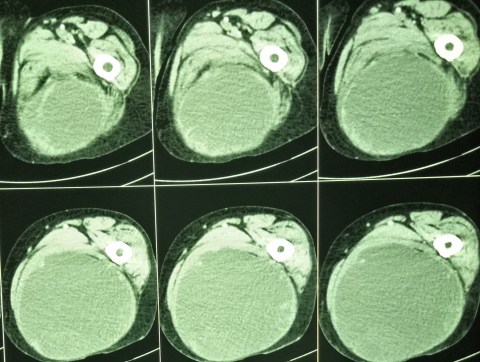
Nephrectomy for a huge renal cell cancer with cystic and solid areas, and with a few stones.

25.1.17
A big ovarian cancer with extensive local spread and ascites.- could only be debulked. (c/o dr Dawra, Fatehabad). However, she had a good response to chemotherapy.
22.2.17
Ileocecal resection and resection for multiple strictures of ileum. 58M (c/o SN in OT). Had been having repeated attacks of obstruction for a few months now. An ileocecal mass locally resected. Several strictures in ileum had to be resected with EEA. A quite proximal stricture in jejunum just bypassed with side-to-side anastomosis. Biopsy revealed tuberculosis.
1.3.17
A ruptured mucocele of appendix. 50 years old female , hospital employee. She was admitted with an appendix mass more than two months back and discharged. However, the appendix mass persisted and a few collections developed in the abdomen. These collections were aspirated and an appendiceal mucocele excised at laparotomy, along with excision of a well localised collection in the pelvis.
Disastrous summer vacation this time (1 july to 31 july)
6.7.16 Had a fall at home (tripped while coming out of the bathroom) at around midnight and fractured the neck of right femur. This was fixed with 4 cannulated screws (zimmer) the next day (7.7.16).
The healing time for this fracture is very long (up to 6 months) and the convalescence painfully slow but if one is lucky and remains active and in a positive frame of mind, it does heal in 3 months time. Mine is healing slowly and I am able to walk with a cane or a walker with partial weight bearing on the leg now.
Three and a half months after the fracture, the x-ray picture was considered satisfactory.

Some earlier stories
23.5.16
Binu joined MD course in DMC Ludhiana, having shifted from paediatrics which she had joined already ( and found it too stressful!). Saw Dr Bajwa (HOD) there and had some nice time with him after so many years.
28.5.16
A lesson relearnt. A failed lap appy converted to find a surprise. The thick and short appendix actually hid a small hard growth in the caecum. A right hemicolectomy was done. Cut section showed a stenosing growth.
19-20 june: conducted the PG surgery exam as internal examiner along with other examiners.
29.6.16
Incisional hernia (following TAH through transverse incision!), repaired with mesh the defect through the right side of the incision. Patient an MD anesthesia herself (Dr Parminder from Sangrur CH).
Rectosigmoid cancer
Posted on: May 18, 2016
18.5.16
A huge ovarian cyst of the right ovary (with very little ovarian tissue salvageable) removed laparoscopically (Dr Karnail Singh’s case).
A rectosigmoid cancer resected by assistant professor Dr Walia, and specimen nicely photographed by a final year medical student.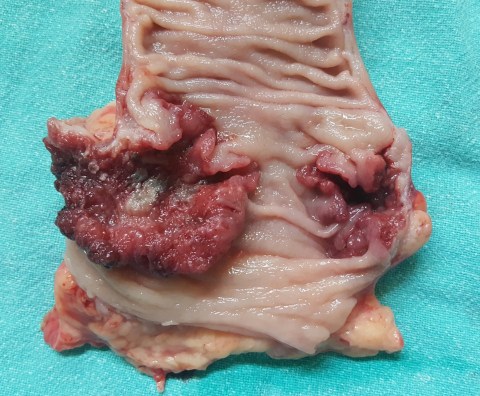
Familial adenomatous polyposis, a huge pseudocyst of pancreas and a choledochal cyst
Posted on: May 17, 2016
5.1.16 to 18.1.16 winter vacation
19.1.16: Following court orders, rechecked theory papers of PG students (who had failed and challenged their failure in court) at BFUHS, Faridkot along with dr Sushil Mittal.
28.1.16 court evidence at Amloh following the issuance of arrest warrants rather than the usual summons for expert witness.
24.2.16
A huge pseudocyst of pancreas in a 25 years old male, proved not to be a cystic neoplasm on investigations, managed by cystojejunostomy Roux-en-Y. The cyst was in the body and tail of pancreas, and parts of its wall had become gangrenous, and had to be excised.

5.3.16
An attempted TEP repair for bilateral inguinal hernias had to be converted to open due to poor relaxation and loss of space.
19.3.16
A choledochal cyst in a 55 years old female, managed by cyst excision and Roux-en-Y hepaticojejunostomy. An anastomotic leak developed and persisted for a long time.
9.4.16
Lap chole in a 62 years old retired doctor (sister of dr Bali, director health and family welfare, Punjab). Thick-walled gallbladder packed with stones. A cholecystohepatic duct appeared high up near the fundus, and was ligated as well as clipped.
12.4.16: Attended court at Dhuri, again following issuance of arrest warrants!

14.5.16
Total proctocolectomy and permanent ileostomy in a 42 years old poor man who had presented with rectal bleeding and severe anaemia, corrected by several blood transfusions. He had a family history of colorectal polyps and also had a duodenal polyp. The distalmost polyps were big and bleeding and possibly malignant and were present in the lower rectum, hence the decision to remove all of distal rectum and anus as well. An abdominoperineal resection and closure of anus were performed after total proctocolectomy was completed.


16.11.15
Multiple big fibroids in a 50 years old lady, causing pain and bleeding. Patient an unmarried jovial lady, and a close friend of Dr Geetanjali. Removed at a total abdominal hysterectomy (patient’s logical choice). She was in Dr Geetanjali’s office a few months later and while we were discussing fibroids remarked happily: “I had the mother of fibroids!”

18.11.15
A distal radical gastrectomy in a 60 years old man (chronic smoker for a long time) for distal cancer causing gastric outlet obstruction. The tumor turned out to be bigger than expected (CT had only reported wall thickening of 2 cm), breaking through serosa and involving multiple lymph nodes above and below the pylorus, besides adhesions posteriorly with the pancreas. 



