Author Archive
24.12.24
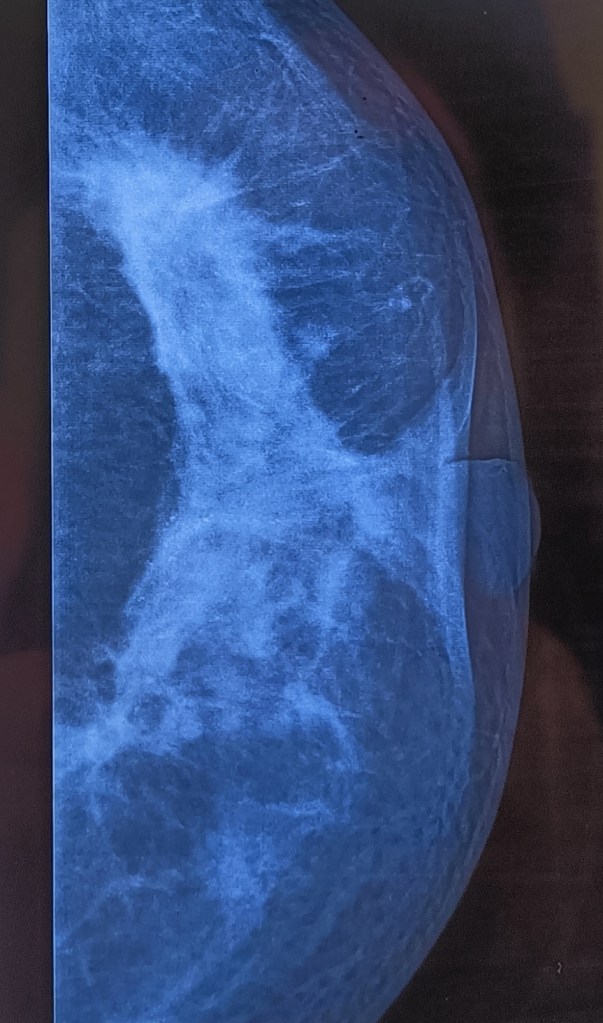
A 42 years old female from Chouhat presented with undiagnosed firmness of the breast which she had noted. Her mother had earlier been treated for breast cancer in our unit more than 25 years earlier. On examination, the nipple retraction was obvious, but FNAC had reported no malignancy. This was perhaps because on palpation no discrete hard mass (as one would find typically) was palpable and so the needle missed the target.

8.12.24
A 66-year-old female was admitted on 6.12.24 with severe abdominal pain and some distension. X-ray showed multiple air-fluid levels.

CT scan the next day showed SBO at mid-level.

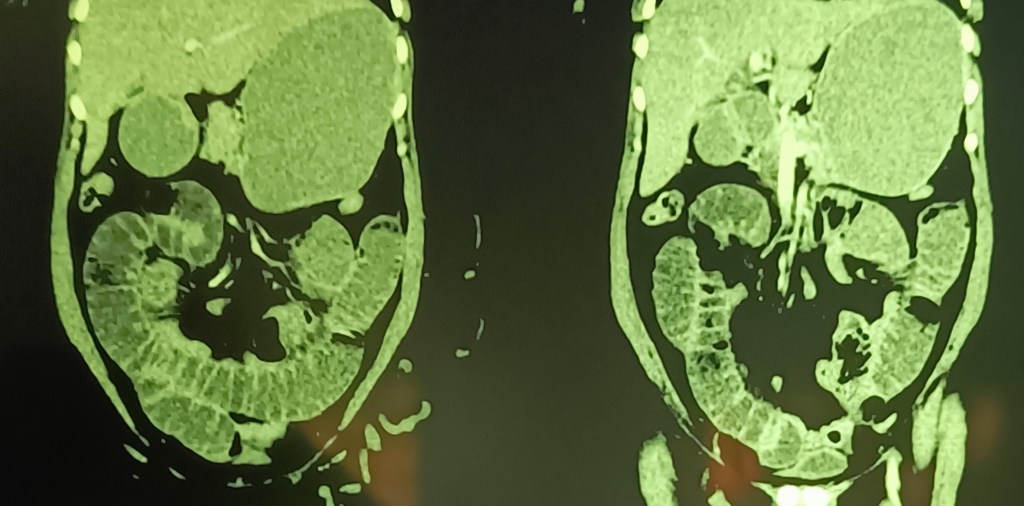
Soon after the CT, the patient’s condition had rapidly improved, with resolution of all symptoms. Neither the patient nor her consultant physician wanted surgery, and so had to withhold the knife, and the patient was discharged.
Constipation can kill too
Posted on: January 3, 2025
17.9.24
The sad and unfortulate story of Amarjit Singh
A 63-year-old male was operated at some private hospital (laparotomy) on 20-6-2024 for massive pneumoperitoneum on abdominal X-ray. The CT on 19.6.24 had shown massive air in peritoneal cavity, slight wall thickening of proximal jejunal loops, a loaded right colon, and the left colon fluid filled and with a wall thickness of up to 10 mm. At laparotomy, the surgeon had found no perforation, but a dilated left colon full of fecal matter and gas which was removed by the rectal tube, and he was prescribed laxatives for constipation; the discharge slip ,mentioning the possibility of a sealed perforation, and a possible diagnosis of toxic megacolon. Was brought to me in a very emaciated condition after the sutures had been removed. However, he still reported that he is constipated, and his abdomen was still found to be distended. A detailed history taken at this time revealed that he was constipated since childhood and has been taking pink tablets (phenolphthalein) regularly for constipation. The treating hospital did make efforts to make a diagnosis with colonoscopy (9.7.24) which showed a small ulcerated nodule 10 cm from anal verge, and later on 23.7.24 a barium enema showed a hugely distended left colon. His general condition continued to worsen, he lost all appetite, became depressed and stopped eating because he did not feel like eating. I could only prescribe regular enemas besides all sorts of other laxatives for him, but he did not improve and eventually died on 17.9.24.
This was a shocking and tragic experience when a patient with possibly congenital constipation which he had been managing with laxatives (phenolphthalein) all his 60 plus years suddenly landing up with acute abdominal pain and distension needing a laparotomy, and his constipation still could not be managed even after operation despite all sorts of medications for constipation and enemas.


A literature search came up with just one report of two cases dying of constipation (Constipation can be deadly. Canadian family physician, vol 38, oct 1992). It concluded that a digital rectal examination can be normal, because stool remains impacted high up, manual disimpaction may not be sufficient and so more is needed. It recommended vigorous use of enemas, and laxatives/osmotic agents orally. However, we tried all these till the end, without success.
18.8.24
A 35 years old female presented with pain RUQ, and found, on ultrasound scan, to have a 1.5 cm stone in the residual gallbladder (h/0 lap chole 2.1.2020) which was smaller and rotund in shape. During the previous operation, the patient had some symptoms 10 days after LC, and found to have a 45-60 ml collection, which resolved with time. At operation, there were dense omental adhesions with the liver in the gallbladder fossa. After this area was cleared, a small residual gallbladder was found with a stone inside. The stone was first removed and the Calot’s triangle cleared to define the CA and CD with difficulty.


30.7.24
All lab investigations and the ultrasound scan were normal in a 50-year-old male presenting with pain and local tenderness over McBurney’ point. The tenderness was exquisite and included some rebound tenderness. At operation, the appendix (preileal in position) presented itself in the wound before even before the cecum could be visualized.
lesson – the most important part of making a diagnosis of acute appendicitis remains proper history and clinical examination rather than labs and scans.
Gall bladder empyema in a 17 years old young man – No lap chole should be taken as easy until after the procedure
Posted on: November 26, 2024
15.7.24
A difficult lap chole had to be performed in a 17 years old young man with acute cholecystitis. At operation, thick pus had to be aspirated to grasp the fundus, and thereafter the stone had to be disimpacted to make dissection easier. Even then the cystic duct junction with the bile duct could not be defined. The gallbladder neck was just ligated under the H. pouch and gallbladder removed.
13.6.24
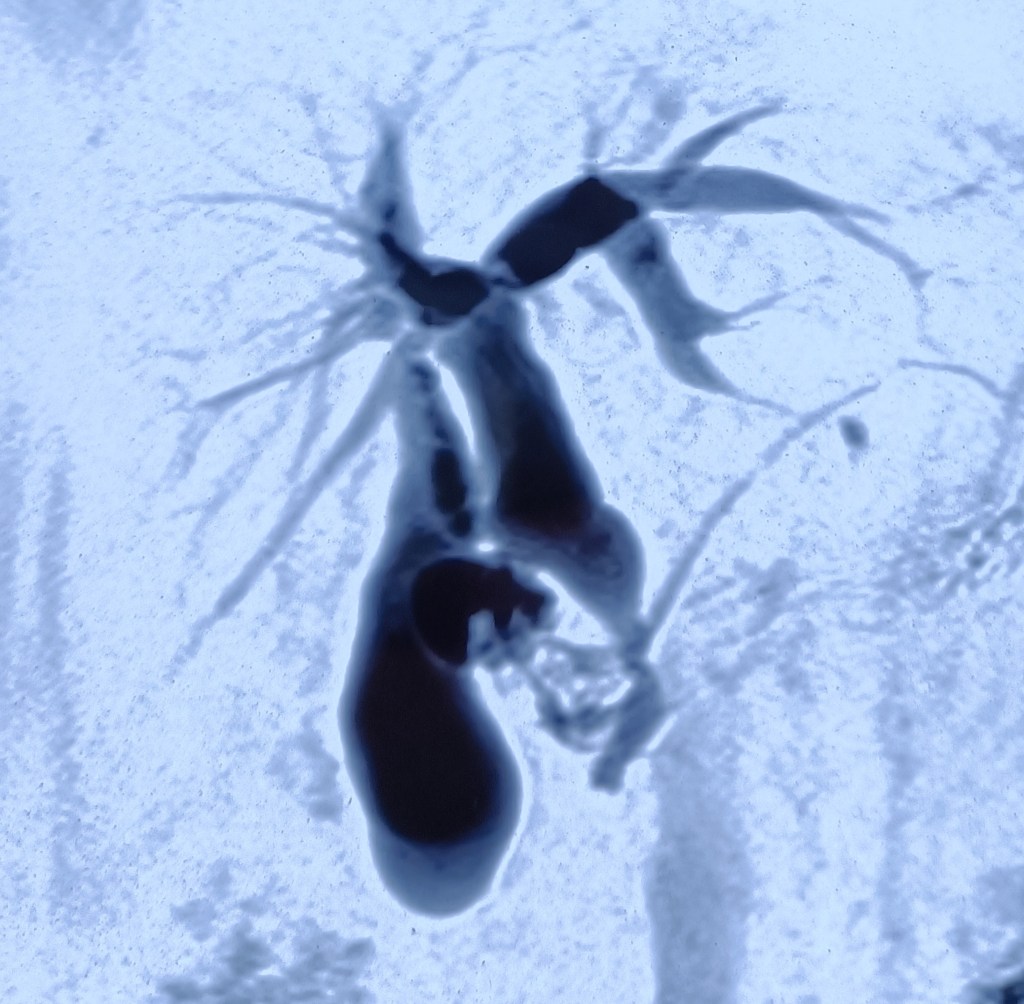
A 65 years old female (Labh Kaur c/o Gurmukh Singh, ex employee RHP) presented with pain in the upper abdomen and fever for the last 15 days, and a tender palpable gallbladder. Her TLC was 16800 with 82% neutrophils. Recovered with antibiotics. LFTs were within normal limits. US and CT showed a dilated gallbladder and dilated EHBD system with CBD of 20 mm diameter, with circumferential thickening of its wall. The CT also reported a narrow intrapancreatic CBD. Suspecting an obstructive pathology (Ca head of pancreas), she was referred to PGI where she was investigated extensively. The pancreas did not have any tumor, and the CA 19.9 was 5.2 (within normal limits). The MRCP reported proximally dilated (16 mm diameter) CBD with short segment of tapering at the level of its junction with pancreatic duct. The junction of PD and BD was seen outside the duodenal wall in the head of pancreas, with the formation of a common channel of length 1.8 mm suggesting pancreaticobiliary maljunction. The common channel was also reported to be prominent in caliber (8 mm diameter). Since her symptoms had already resolved with a short course of antibiotics, she was sent home, to be just observed in the future for any recurrence of symptoms.
22.5.24
A twenty five years old tall (just more than 6 feet) young man from the local jai jawan colony had acute calculus cholecystitis, was treated with antibiotics for a week, and recovered.
At operation, found to have a very thick walled empyema, which took nearly 4 hours to complete laparoscopically.
Difficulties as usual: the omental adhesions took half an hour to clear the gall bladder. Then the fundus grasp being impossible, the gallbladder was opened up by a vertical bisection, and all stones removed from within it including the one impacted in the H pouch – picking up and removing all these stones one by one. All this took more than one hour. The grasp now being possible at fundus and H pouch, the thick walls of the big gallbladder were removed from both sides (to make it more manageable), and the gallbladder transected just above the H pouch. Dissecting behind the pouch now it was possible to make space behind it so as to pass a no 1 vicryl suture behind and ligate it just below the H pouch. As all this is done very slowly and carefully, it consumed more than one hour. The remaining gallbladder was now removed leaving some of the posterior wall alone.
Post-operatively the patient recovered very nicely and quickly and sent home in the evening.
To contrast with this, in the similar case (4 hours) done last month (19.4.24), it was not possible to make a safe space behind the gallbladder/H. pouch to pass a ligature; the fibrosis of the area was so dense (the real frozen Calot’s triangle). Hence, the case was converted to open, and a right-angle clamp used to make that space, resulting in a close shave with the underlying CBD, exposing its mucosa. Bile leak continued through the drain for nearly 3 weeks and then dried up.
4.5.24
An elderly patient (c/o Gurmukh Singh, ex-employee, gynae), 70 years of age, presented with epigastric and RUQ symptoms, with previous history of open cholecystectomy 2 years back at Malerkotla civil hospital through a small incision (so-called mini-lap).

The ultrasound scan, however, still showed a smaller rounded gallbladder.
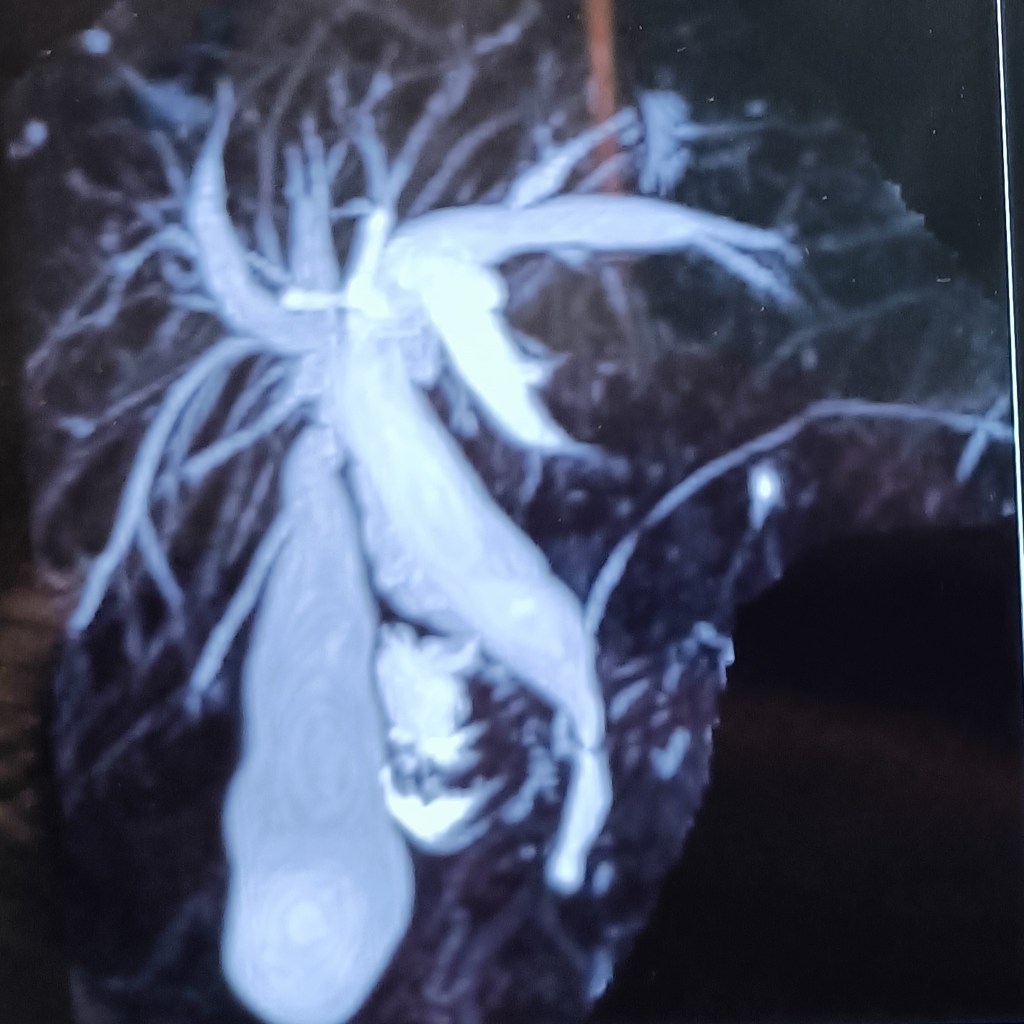
An MRCP was obtained for local biliary anatomy.

At lap chole, dense omental and colonic adhesions took time to safely dissect off the top of the gallbladder which came into view only at the middle of the gallbladder fossa.
Thereafter, the going was easy. It was a small rotund residual gallbladder, suggesting the upper half had been removed (partial cholecystectomy).
